Measles: The Disease, The Vaccine and The Global Impact
Explore our comprehensive guide on Measles, a highly contagious disease that can lead to severe complications. Learn about its symptoms, transmission, and the importance of vaccination in preventing its spread. Understand the risks, especially for children and adults with compromised immune systems, and the global efforts to eliminate this disease. Stay informed and protect your health.
1) Introduction
Hello there, dear readers! Welcome to our blog,
where we delve into the intriguing, and at times befuddling, world of health
and wellbeing. Today, we're going to look at an issue that's been making news
all around the world: measles.
The measles virus (MV) causes the extremely
infectious condition known as rubeola. With 21 distinct strains known to exist,
this virus is a bit of a shape-shifter. It's a little like a comic book
villain, constantly shifting shape to avoid capture. But don't worry, our
scientists and healthcare specialists are constantly on the case!
This is no easy sickness to deal with. It
appears to begin innocently enough, with symptoms such as a high temperature,
cough, and runny nose. Then it shows its real hues. A rash appears at the
hairline and spreads downhill to cover the majority of the body. Not to mention
the little white dots known as Koplik's spots, which form inside the mouth.
The measles virus is an expert at concealment
and invasion. It infects the host by binding to host-specific receptors via its
H and F proteins. It acts like a miniature Trojan horse, deceiving our cells
into allowing it to enter. Once inside, it multiplies rapidly, wreaking damage
on our bodies.
But here's the catch: Measles can be avoided.
Yes, you read that correctly. We have the ability to halt the spread of this
illness. Our defense against this invader is the measles, mumps, and rubella
(MMR) vaccination, which is around 97 percent effective at preventing measles
after two doses.
Despite this, measles remains a global issue,
killing over 100,000 people each year. What's the reason? Lower vaccination
rates in some communities, making more individuals susceptible to the disease
and diminishing herd immunity.
So, dear readers, let us arm ourselves with
information and act. Let us guarantee that we and our loved ones are immunized.
Let us spread the word about the need of vaccination not only for our own
health, but also for the health of our communities. Stay tuned for future pieces
that will go deeper into the realm of measles. We'll look at the disease's
science, the need of immunization, and much more. We can make a difference if
we work together. Welcome to our exploration of the world of measles!
The earliest recorded record of measles in the
United States was made in 1657 by a Boston, Massachusetts resident. By the
early twentieth century, measles was responsible for around 6,000 fatalities
each year in the United States. Prior to the introduction of a vaccine,
virtually all children had measles by the age of 15, resulting in an estimated
3 to 4 million cases in the United States alone per year.
The discovery of a vaccine in the mid-twentieth
century was a watershed moment in the history of measles. During a measles
outbreak in Boston, Massachusetts in 1954, John F. Enders and Dr. Thomas C.
Peebles identified the virus. They developed a vaccine using this strain,
called as the Edmonston-B strain. The first measles vaccine was licensed for
general use in 1963 after successful testing. In 1968, an enhanced version of
the vaccine was introduced.
The advent of the measles vaccination resulted
in a considerable decrease in the disease's incidence. The Centers for Disease
Control and Prevention (CDC) established the aim of eradicating measles in the
United States in 1978. Although the target date was not realized, widespread
use of the measles vaccination significantly decreased illness rates. By 1981,
the number of reported measles cases had dropped by 80% from the previous year.
Measles was declared eradicated in the United States in 2000, indicating that
there had been no continuous disease transmission for more than 12 months. This
was a remarkable accomplishment made possible by the United States' extremely
effective immunization program and enhanced measles control in the Americas
area.
However, the battle against measles is far from
done. Despite the availability of a highly effective vaccine, measles outbreaks
continue to occur, particularly in low-vaccination-rate regions. These
outbreaks highlight the critical significance of maintaining high vaccination
coverage in order to prevent the recurrence of this potentially lethal illness.
Finally, the history of measles demonstrates
the power of scientific discovery and public health action. Measles, which was
formerly a prevalent and frequently fatal illness, has been almost eradicated
because to the invention and widespread use of a vaccination. The ongoing
occurrence of outbreaks, on the other hand, serves as a reminder of the need of
vaccination in limiting the spread of this extremely dangerous illness.
Prior to the 1963 release of the measles
vaccine, significant outbreaks occurred every two to three years, resulting in
an estimated 2.6 million fatalities per year. Despite the availability of a
safe and cost-effective vaccine, a projected 128,000 individuals died from
measles in 2021, the majority of whom were children under the age of five.
Accelerated vaccination efforts by governments,
WHO, and other international partners averted 56 million deaths between 2000
and 2021. Measles mortality reduced from 761,000 in 2000 to 128,000 in 2021 as
a result of vaccination.
More than 140,000 people died from measles in
2018. The vast majority of measles deaths (more than 95%) occur in nations with
poor per capita incomes and inadequate health-care facilities.
Measles immunization avoided 17.1 million
deaths globally between 2000 and 2014, a 79% reduction. Measles is expected to
infect 9 million individuals worldwide by 2021. For more than 50 years, safe
and effective vaccinations against measles and rubella have been available.
Between 2000 and 2021, measles immunizations saved more than 56 million lives
globally.
The average number of measles cases recorded in
the United States every year was 130. The vast majority of case-patients from
the United States were unvaccinated (74%). In the United States, it is
predicted that 9,145,026 children (13.1%) are vulnerable to measles. If no
attempt is made to catch-up with pandemic vaccination rates, 15,165,221
youngsters (21.7%) will be vulnerable to measles.
Global coverage with regular first-dose MCV
(MCV1) grew from 72% to 85% between 2000 and 2019.
These figures emphasize the need of maintaining
and boosting vaccination rates in order to prevent the spread of measles and
minimize the number of fatalities caused by the illness.
2) Measles
Virus
a) Classification and Structure of Measles
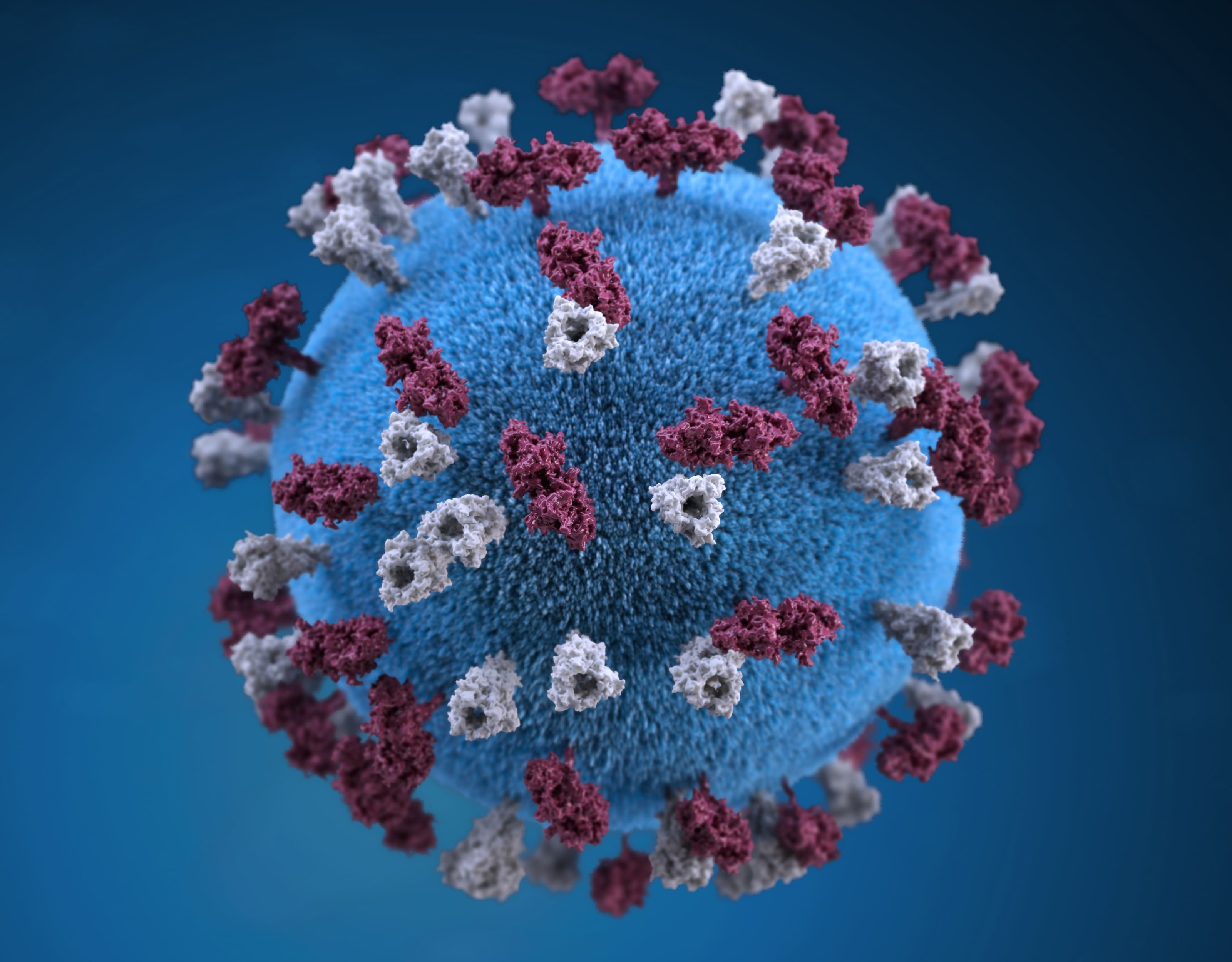
MeV is a member of the Morbillivirus genus,
which is part of the Paramyxoviridae family. The Paramyxoviridae family has two
subfamilies: Paramyxovirinae and Pneumovirinae. The subfamily Paramyxovirinae
is further subdivided into seven genera. The genome of the measles virus is
generally 15,894 nucleotides long and encodes eight proteins. The World Health
Organization (WHO) presently recognizes eight measles clades (A-H), with 23
subtypes.
On the viral surface, there are two envelope
glycoproteins: hemagglutinin (H) and membrane fusion protein (F). These
proteins are in charge of binding to host cells and invading them. The H
protein is responsible for receptor attachment, while the F protein is
responsible for viral envelope and cellular membrane fusion. Furthermore, the F
protein can induce infected cells to directly merge with nearby uninfected
cells, resulting in the formation of syncytia.
b) Genome and Proteins of Measles
The genome of the measles virus is generally
15,894 nucleotides long and encodes eight proteins. The WHO presently recognizes
eight measles clades (A-H). Subtypes are denoted by numerals such as A1, D2,
and so on. There are now 23 identified subtypes.
P, an important polymerase cofactor, and V and
C, which have many activities but are not absolutely necessary for viral multiplication
in cultured cells, are encoded by the measles virus (MV) P gene. The V protein
is not connected with intracellular or released viral particles and is
translated from an altered P mRNA.
c) Pathogenesis and Transmission of Measles
Measles is a very infectious illness spread by
respiratory aerosols. The virus first infects CD150+ lymphocytes and dendritic
cells in circulation and lymphoid organs, then spreads to nectin-4 expressing
epithelial cells.
In previously uninfected humans and nonhuman
primates, the virus produces systemic illness. Measles is marked by fever and a
skin rash, as well as cough, coryza, and conjunctivitis. The transitory immune reduction
caused by measles makes people more susceptible to opportunistic infections.
Measles is so contagious that if one person
gets it, up to 90% of those in close proximity who are not immune will also get
it. Infected persons can infect others four days before and four days after the
rash emerges. After an infected individual leaves a location, the measles virus
can survive in the air for up to two hours.
3) Clinical
Features of Measles
Rubeola, or measles, is a highly infectious
viral virus that predominantly affects youngsters. It is distinguished by a
widespread skin rash and flu-like symptoms. The major location of infection in
the lungs is alveolar macrophages or dendritic cells. The measles virus travels
to regional lymphoid organs after initial replication in the lung, resulting in
systemic infection.
a) Symptoms and Signs of Measles
Measles symptoms usually occur 10 to 14 days
after being exposed to the virus. A high fever, cough, runny nose, and red,
watery eyes (conjunctivitis) are the first signs. Koplik's spots, which are
small white spots that may form within the mouth two to three days after the beginning
of symptoms, are frequently associated with these symptoms.
A rash generally appears three to five days
after the initial symptoms, appearing as flat red patches on the face at the
hairline and extending downhill to the neck, torso, arms, legs, and feet. On
top of the flat red dots, little raised bumps may form. As the spots travel
from the head to the rest of the body, they may become connected. When the rash
occurs, a person's temperature may reach 104° Fahrenheit.
b) Incubation Period for Measles
The incubation period for measles, which is the
time between exposure and the development of symptoms, is 11 to 12 days on
average. The average duration between exposure and rash start is 14 days, with
a range of 7 to 21 days. The measles virus spreads in the body throughout the
incubation period, although there are no signs or symptoms of measles.
Measles complications can be severe, especially
in children under the age of five, individuals over the age of twenty, pregnant
women, and those with impaired immune systems. Ear infections and diarrhea are
common problems. Severe problems include pneumonia (lung infection) and
encephalitis (brain swelling), which can result in hospitalization and even
death.
One in every five unvaccinated persons in the
United States who contract measles is hospitalized. Pneumonia, the most
prevalent cause of mortality from measles in young children, affects as many as
one out of every twenty children infected. One in every 1,000 children who have
measles will develop encephalitis, which can cause convulsions and leave the
kid deaf or intellectually disabled.
Long-term effects of measles include subacute
sclerosing panencephalitis (SSPE), an extremely rare but devastating central
nervous system condition caused by an earlier measles virus infection. SSPE
often occurs 7 to 10 years after a person has measles, even if the person
appears to have recovered completely from the infection.
4) Clinical
Diagnosis of Measles
Measles is an acute viral respiratory infection
marked by a fever and malaise prodrome, cough, coryza, and conjunctivitis,
generally known as the three "C"s. A maculopapular rash follows a
pathognomonic enanthema, Koplik dots. The rash typically starts 14 days after
exposure and progresses from the head to the trunk to the lower limbs. Patients
are infectious from four days before to four days after the rash emerges.
Immunocompromised people may not get the rash at all.
The disease's distinctive rash, as well as a
tiny, bluish-white patch on a bright red backdrop — Koplik's spot — on the
inside lining of the cheek, may typically be used to identify measles. The
provider may inquire if you or your kid has had measles immunizations, whether
you have recently gone abroad outside of the United States, and if you have had
contact with somebody who has a rash or fever.
a) Laboratory
Confirmation of Measles
All sporadic measles cases and outbreaks
require laboratory confirmation. The most popular procedures for confirming
measles infection are the detection of measles-specific IgM antibody in serum
and measles RNA by real-time polymerase chain reaction (RT-PCR) in a
respiratory samples. At the time of first contact, healthcare practitioners
should collect a blood sample as well as a throat swab (or nasopharyngeal swab)
from individuals suspected of having measles. Urine samples may also contain
the virus, and collecting both respiratory and urine samples, when possible,
might improve the probability of identifying the measles virus.
b) Serologic Testing for Measles
The presence of particular IgM antibodies in a
serum samples taken during the first few days of rash development can give
presumptive proof of a current or recent measles virus infection. However,
because no assay is 100% specific, serologic testing of non-measles patients
using any assay may provide false positive IgM findings on occasion. Serologic
tests can potentially provide false-negative results if serum specimens are
taken too soon after the commencement of the rash.
Both IgG and IgM antibodies develop within 3-7
days of the commencement of a primary infection. Both antibodies then rise
until they reach a plateau 2-3 weeks later. Antibody levels can be reported as
Non-Reactive (no detectable antibody), Indeterminate (the degree of antibody
observed is borderline reactive or equivocal), or Reactive (the antibody is
detectable within the assay's positive range).
c) Genotyping of Measles Virus
During epidemic investigations, measles viral
genotyping can be useful in tracking transmission paths. The findings of
genotyping can assist confirm, deny, or uncover links between instances. If two
instances contain identical N-450 sequences, they may be linked even if the
link is not clear. Measles virus genotyping can also assist determine which
foreign country is responsible for an imported case in the United States.
However, genotyping alone is insufficient since one genotype might exist in
several nations and even parts of the world. To establish whether nation may be
the source of an imported US case, genotype data should be analyzed in
conjunction with epidemiological information such as travel and exposure histories.
5) Epidemiology
of Measles
Measles is a contagious viral illness that was
originally reported in the seventh century. Prior to the availability of a
vaccine, measles virus infection was practically ubiquitous during infancy, and
more than 90% of people were immune due to previous infection by the age of 15
years. In underdeveloped nations, measles is still a frequent and often fatal
disease. According to the World Health Organization, there were 142,300 measles
fatalities worldwide in 2018.
Measles is a highly infectious virus that
dwells in the mucus of an infected person's nose and throat. Coughing and
sneezing might transmit it to others. Other individuals can become sick if they
breathe contaminated air or contact an infected surface and then touch their
eyes, noses, or mouths. Infected persons can infect others four days before and
four days after the rash emerges. After an infected individual leaves a
location, the measles virus can survive in the air for up to two hours.
b) Temporal Pattern of Measles
The seasonality of measles varies by area. In
Guangxi, China, for example, seasonal maxima occurred between April and June,
and a temporal measles cluster was found in 2014. Overall, a two-piecewise
temporal pattern of measles incidence was detected during the whole 11-year
period, with a decrease from 2004 to 2009 and an upswing from 2010 to 2014.
c) Secular Trends in the United States for Measles
Prior to 1963, the United States recorded
roughly 500,000 cases and 500 measles fatalities each year, with epidemic
cycles occurring every 2 to 3 years. However, the true number of cases is
believed to be between 3 and 4 million every year. More than half of people had
measles by the age of six, and more than 90% had it by the age of fifteen.
Measles incidence plummeted by more than 95% in the years after the vaccine's
approval in 1963, and 2- to 3-year epidemic cycles were no longer common. In
2019, 13 measles outbreaks were recorded, accounting for 663 cases; six of
these outbreaks were connected with underimmunized close-knit groups,
accounting for 88% of all cases.
Measles outbreaks continue to occur as a result
of the disease's high contagiousness and the existence of unvaccinated
populations. The most recent epidemic in the United States occurred in 2019,
largely among unvaccinated persons. Outbreaks can also develop in areas with
unvaccinated populations. For example, in 2015, a measles epidemic occurred at
a child care center in Illinois, when virtually all of the unimmunized infants
under the age of one year caught the disease. Globally, measles epidemics can
cause serious complications and fatalities, particularly in young, malnourished
children. Cases imported from other countries continue to be a major source of
infection in nations nearing measles eradication.
6) Surveillance
and Reporting for Measles
Surveillance and reporting are critical
components of public health, especially when it comes to infectious illnesses
like measles. Surveillance is the continuous collecting, analysis, and
interpretation of health data, which is required for planning, executing, and
evaluating public health initiatives. Measles cases in the United States are
reported to the Centers for Disease Control and Prevention (CDC) via the
National Notifiable Diseases Surveillance System (NNDSS) by states. Every
confirmed measles case should be subjected to active monitoring to ensure
prompt reporting of suspected cases in the population.
As the number of measles cases declines, so
does the need of monitoring. As a result, a thorough laboratory analysis of
probable measles cases is a critical component of measles eradication
initiatives.
a) Case Identification for Measles
Case detection is an important stage in disease
surveillance. It entails identifying and documenting probable cases of a
disease. A clinical case definition has been devised in the context of measles
to help in identification. Anyone with a fever, widespread maculopapular
(non-vesicular) rash, cough, coryza (runny nose), or conjunctivitis (red eyes)
is suspected of having measles. The distinction between imported and indigenous
cases becomes increasingly significant when the success of stopping indigenous
measles transmission is measured. Identifying suspected measles patients is
critical during a measles eradication campaign, especially given the low
clinical suspicion of measles.
b) Data Collection for Measles
Data gathering is an essential component of
monitoring and reporting. It entails obtaining extensive information about each
patient, such as demographics, clinical symptoms, immunization history, and so
on. The information gathered is utilized to confirm measles cases, including
critical clinical information such as the date of beginning of symptoms, date
of sample collection, and measles vaccination history necessary. During case
investigation, the measles surveillance worksheet should be used as a guideline
for gathering demographic and epidemiologic data. Surveillance data is also
used to summarize current measles epidemiology and to evaluate preventative
programs and attainment of goals such as disease eradication.
c) Reporting Procedures for Measles
When a case is discovered and data is gathered,
it must be reported to the proper health authorities. In the United States,
measles cases should be reported to the CDC as soon as possible (within 24
hours) by the state health department. Measles, for example, must be reported
to the Minnesota Department of Health (MDH) 24 hours a day, seven days a week.
State legislation requires health care practitioners, health care institutions,
medical labs, and, in some cases, veterinarians and veterinary medical
laboratories to report disease to the health department. The reporting of measles
cases is critical for tracking the disease's transmission, adopting control
measures, and assessing the efficacy of preventative programs. It is also
critical for maintaining public and health-care professional awareness.
7) Prevention and
Control of Measles
The primary means of preventing and controlling
the spread of measles is to ensure community vaccination. The measles
vaccination, which is frequently delivered as part of the MMR vaccine, is the
most effective strategy to prevent the disease. The Centers for Disease Control
and Prevention (CDC) advises that children take two doses of the MMR
vaccination, the first at 12 to 15 months and the second at 4 to 6 years. Teens
and adults should also have their MMR immunizations up to date. Aside from immunization,
timely identification and isolation of individuals with known or suspected
measles is critical in limiting disease transmission. This involves following
conventional precautions including airborne precautions in hospital
environments.
MMR vaccination is extremely safe and
effective. Two doses of the MMR vaccination are around 97% effective in
preventing measles, whereas one dose is approximately 93% effective. The first
dosage is usually given between the ages of 12 and 15 months, and the second
dose between the ages of 4 and 6 years. The second dose, however, can be
administered as soon as 28 days following the first. Adults born before 1957
are almost always immune since they were exposed to measles as children. Those
born in 1957 or after must have received at least one dose of the MMR
vaccination. Certain populations, including college or university students,
overseas tourists, and healthcare workers, are advised to have two doses of the
MMR vaccination.
b) Post-exposure Prophylaxis for Measles
PEP is a preventative medical treatment that
begins promptly after exposure to a pathogen (such as the measles virus) to
avoid infection or sickness. PEP for measles can be administered as the MMR
vaccination within 72 hours of initial exposure, or as immunoglobulin (IG)
within six days. However, the MMR vaccination and IG should not be given at the
same time, as this renders the vaccine ineffective. The type of PEP used and
the requirement for quarantine are determined by the individual's age,
immunological condition, and time after exposure. Non-immune babies under 6
months of age, for example, should be administered intramuscular immunoglobulin
(IMIG) and isolated at home for 28 days following the previous exposure if it
happened within three days. If the exposure happened during the previous 4-6
days, IMIG should still be administered, but the quarantine time is lowered to
21 days.
c) Isolation
and Precautions for Measles
Patients with known or suspected measles should
be admitted to an airborne infection isolation room (AIIR) right away. If an
AIIR is not available, the patient should be relocated to an institution that
does. In the meanwhile, the patient should be placed in a private room with the
door shut. Patients with measles should use airborne precautions for four days
after the rash appears. Immunocompromised patients with measles should continue
to use airborne precautions for the length of their illness due to extended
viral shedding. In healthcare settings, regardless of presumptive immunity
status, all workers entering the room of a measles patient should employ
respiratory protection consistent with airborne infection control protocols.
8) Measles in
Specific Populations
a) Infants,
Children, and Adolescents
Rubeola, or measles, is a highly infectious
sickness that predominantly affects youngsters. It is caused by a virus and is
distinguished by a widespread skin rash and flu-like symptoms. A hacking cough,
runny nose, high fever, and red eyes are typical of a measles illness. Before
the rash appears, children may have Koplik's spots (little red patches with
blue-white centers) within their mouth. The rash appears 3-5 days after the
symptoms begin, frequently in conjunction with a high temperature of up to
104°F (40°C). Measles is highly contagious, with 9 out of 10 unvaccinated
persons at risk of contracting it if they come into contact with an infected
person. When others breathe in or come into direct touch with virus-infected
fluid, such as droplets blasted into the air when someone with measles sneezes
or coughs, the virus spreads.
The greatest approach to prevent children
against measles is to get them inoculated. Measles protection is included in
the measles-mumps-rubella (MMR) or measles-mumps-rubella-varicella (MMRV)
vaccines given to most children when they are 12 to 15 months old and again
when they are 4 to 6 years old. Approximately 95% of patients gain immunity
after their first immunization, with the remainder developing immunity during
their second vaccination. Immunity is permanent.
Adults over the age of 20 are more prone to get
measles complications. Ear infections and diarrhea are common problems, but
pneumonia and encephalitis are dangerous. One in every five unvaccinated
persons in the United States who contract measles is hospitalized. Pneumonia,
the most prevalent cause of mortality from measles in young children, affects
as many as one out of every twenty children infected. One in every 1,000
children who have measles will develop encephalitis (brain swelling), which can
cause convulsions and leave the kid deaf or intellectually disabled.
Travelers who have not been completely
vaccinated or who have never had measles are at risk of infection if they
travel overseas to regions where measles is circulating. Getting vaccinated is
the greatest method to protect yourself and your loved ones against measles.
You should plan on being completely immunized at least two weeks before your
trip. If your vacation is less than two weeks away and you are not immune to
measles, you should still obtain the measles-mumps-rubella (MMR) vaccination.
Cases of measles in the United States are
caused by unvaccinated overseas tourists. Unvaccinated persons who become ill
in other nations bring the disease into the United States. They can transfer
measles to those who are not immune, which can lead to outbreaks.
To summarize, measles is a highly contagious
illness that can affect people of all ages, but it is most harmful for
newborns, children, adolescents, adults over the age of 20, and unvaccinated
travelers. The most effective strategy to avoid measles and its effects is
vaccination.
9) Real Life
Testimonials and Stories of People who have suffered from Measles
Brenda Shaw had measles as a
four-year-old in 1950, an incident that changed her life forever. The illness
caused her eardrum to break, rendering her deaf in her right ear. This issue
has generated problems that she is still dealing with. Brenda spent a month in
the hospital due to a burst eardrum caused by the measles illness. Despite
having two eardrum transplants, she is still deaf in her right ear. The
infection's consequences frequently lead her to experience dizziness and nausea.
Vertigo, a disorder that creates a spinning sensation or loss of balance, can
be caused by problems in the inner ear or brain. Nausea is a typical side
effect of vertigo.
Brenda's episode of measles was
not a unique one. During the outbreak in 1950, her best friend became sick and
suffered lifelong eye impairment. Another student experienced hearing loss in
both ears. There was no measles vaccination available at the time.
Brenda's personal experience with
the serious consequences of measles has made her a staunch supporter of
immunization. "For God's sake, vaccinate your children," she says,
urging parents to vaccinate their children against measles. It is not the cause
of autism." This comment is in reaction to the widely debunked 1998 study
by Dr. Andrew Wakefield that linked immunizations to autism. In 2010, the
medical publication The Lancet withdrew the report, which was regarded as a
"elaborate fraud" by other researchers.
Measles is one of the most
infectious illnesses on the planet, and it may live in the air or on surfaces
for hours. Even before the rash forms, it can be spread by coughing or
sneezing. Blindness, encephalitis, and severe diarrhea are all serious symptoms
of a measles infection. One in every ten persons infected with the illness may
develop ear infections or pneumonia, and one in every 3,000 will die from
respiratory or neurological problems.
Brenda's experience serves as a
harsh reminder of the disease's potential severity and the need of immunization
in preventing it and its repercussions. Her story emphasizes the importance of
ongoing public health initiatives to maintain high vaccination coverage and to
combat vaccine disinformation.
Maggie's story is a strong
witness to the significance of immunization and the hazards that vulnerable
people face when others refuse to vaccinate. Maggie, a young cancer patient,
was exposed to measles, a highly infectious illness that may be especially
harmful for people with weakened immune systems.
Maggie's father, board-certified
pediatrician Dr. Tim Jacks, revealed their experience in 2015. Maggie was
undergoing cancer treatment at the time, which included many rounds of
chemotherapy, lumbar punctures, and surgery to insert a port. Maggie, while
being completely inoculated prior to her cancer diagnosis, was unable to obtain
more vaccines until her treatments were completed.
The measles exposure happened
during a measles epidemic caused by an unprotected Disneyland visitor. Measles
is very infectious and may live airborne in a room for up to two hours,
infecting someone. It is also contagious four days before the rash begins,
making it difficult to diagnose. Measles complications can be deadly, including
ear infections, diarrhea, pneumonia, brain inflammation, and even death.
On January 21, Maggie and her
younger brother Eli, who was too young to get the MMR vaccine, were exposed to
measles. They had to stay in seclusion until February 11 to prevent the
sickness from spreading. The family had to postpone plans and live in terror of
the emergence of measles symptoms as a result of this predicament, which
created tremendous disruption and worry.
Dr. Jacks is frustrated and angry
with parents who refuse to vaccinate their children. He reminded out that their
decisions effect not just their own children, but also vulnerable youngsters
like Maggie. He underlined the importance of "herd immunity," which occurs
when a large percentage of the population is vaccinated, offering some
protection for individuals who cannot receive particular vaccinations, such as
children. Maggie
Maggie's tale emphasizes the
necessity of immunization in reducing the spread of infectious illnesses and
safeguarding vulnerable members of the community. It also emphasizes the
possible repercussions of vaccination apprehension, which may be caused by a
variety of circumstances, including misinformation regarding vaccine safety and
efficacy.
Measles can be especially
concerning for cancer patients due to their decreased immunity as a result of
therapies such as chemotherapy. While effective immunization has reduced
measles incidence, the illness can still represent a major risk to these
people.
Finally, Maggie's tale serves as
a strong reminder of the vital role immunizations play in safeguarding not just
our own health, but also the health of those around us, especially the most
vulnerable people of our community.
Varya, a three-year-old child
from Kazakhstan, had measles when she was three. Alexei and Nastya Naumov, her
adoptive parents, had adopted her from an orphanage despite her severe
sickness, which had rendered her immunocompromised. They had been instructed
mistakenly not to give her several childhood immunizations, including the
measles vaccine, due to her illness.
Varya got red patches on her legs
in February 2019, which were first identified and treated as an allergic response.
When her temperature reached 40 degrees Celsius, an infectious disease
specialist was summoned. She was then diagnosed with hemorrhagic vasculitis,
which was caused by measles.
Varya was sent to an infectious
disease hospital, where she became seriously ill during the following 10 days.
Nastya, Varya's mother, recounts the terrifying time: "Varya was burning
with a fever, crying from pain at night." Varya grew thin and unable to
swallow, weighing barely 17 kg. Her cognitive abilities were damaged by the
extended high-grade fever, which now affects her ability to do her schoolwork.
Varya was in the hospital for six
and a half weeks. The hospital was packed with children and adults suffering
from measles throughout her visit. Nastya still gets upset when she thinks of
Varya's measles struggle, saying, "How would you feel if you saw your
child suffer so much?" "I'm at a loss for words."
In 2019, Kazakhstan had a measles
epidemic with 13,326 cases. Of the 9,409 measles cases reported among children
aged 0 to 14, 7,802 (83%) were unvaccinated. Many were infants who were too
young to receive the measles vaccine. However, vaccination rejection accounted
for 22% of the unvaccinated, while medical contraindications (both genuine and
imagined) accounted for 30%. Unfortunately, the sickness claimed the lives of
nineteen children and two adults.
Varya's trauma occurred about two
years ago, and she is now inoculated and protected against several avoidable
diseases. She has had no bad reactions to any of the immunizations she has been
given.
Varya's tale emphasizes the
significance of immunization, especially in safeguarding vulnerable people like
her. It also emphasizes the possible implications of vaccine misinformation and
the importance of correct vaccination guidance and education.
Cecilia Rodriguez, a Houston
resident, caught German Measles when she was 13 months old, 30 years ago. Her
father, Carlos, first assumed she had a cold because of symptoms such as fever
and a runny nose. Her health immediately deteriorated, and she became unable to
breathe, prompting her parents to hurry her to Texas Children's Hospital.
Cecilia was in a coma for nine
months as a result of the measles virus, during which she underwent many
life-saving but risky procedures. Her speech, hearing, and eyesight were all
affected by the sickness, which had a significant influence on her life. As a
result, she was in special education courses for several years.
Measles is a hazardous disease
that can cause serious consequences such as pneumonia and encephalitis (brain
swelling). These issues might lead to hospitalization and even death in extreme
circumstances. Indeed, roughly one in every three infants infected with measles
will die from respiratory and neurologic problems.
In Cecilia's instance, she was
also advised that the condition would most likely prevent her from having
children. She bucked these expectations, however, and is now a mother of three
children. Cecilia did not give up despite the difficulties she experienced. She
completed her education and volunteered extensively.
Cecilia's measles experience
emphasizes the disease's possible long-term consequences. According to
research, measles can induce long-term immune system damage, resulting in a
type of immunological amnesia that can put children at risk of sickness from
other infections for years. This is due to the fact that the measles virus can
cause a considerable loss of antibodies, which are essential for combating
diseases. It might take 2 to 3 years for the immune system to recover after a
measles infection.
Cecilia's tale emphasizes the
significance of immunization in the prevention of measles. The MMR (measles,
mumps, and rubella) vaccine was not administered to Cecilia until she was 15
months old. Following the 1989 outbreak, which infected 3,200 Texans, the
medical community reduced the age to 12 months. Cecilia now guarantees that all
of her children are vaccinated and up to date because she does not want them to
go through what she did.
Muhammad Ghafoor, a Pakistani
worker, was traumatized when his ten-month-old son, Muhammad Rahim, acquired
measles and was taken to the critical care unit at Benazir Bhutto Hospital's
Paediatric Department in Rawalpindi, Pakistan. Rahim's health was grave, and he
had been on the verge of dying for 14 days.
Rahim first had measles, which
lowered his immune system, and then he got pneumonia. Ghafoor and his wife,
Safina Jan, had first taken Rahim to a government hospital for the first few
prescribed vaccines. However, their dedication waned with time, and they
ignored the measles vaccination, which is generally given to kids at the age of
nine months. As a result, when a measles outbreak arose, Rahim was helpless.
Ghafoor confesses that the
underlying reason of his son's life-threatening sickness was his lack of
information about the need of immunization. He had dismissed immunization as a
minor duty. This lack of knowledge and misunderstandings regarding
immunizations is frequent among low-income and educated households in Pakistan.
Despite huge vaccination
campaigns, measles remains a substantial concern for the unprotected in
Pakistan. According to provincial health officials, eleven children died from
measles in the Rawalpindi district of Pakistan's Punjab province between
January and May, while hundreds were confirmed to be afflicted.
Dr. Mukhtar Ahmed Awan, Director
of Punjab's Expanded Immunization Program, stated that measles is skilled at
exploiting even minor immunity deficiencies. Seven of the 11 children who died
of measles in Rawalpindi were completely unimmunized, while the others had only
gotten a single dosage of the two-dose regimen.
Ghafoor's and his family's story
emphasizes the necessity of immunization in preventing potentially fatal
diseases like measles. It also emphasizes the significance of greater
vaccination awareness and education, particularly in low-income and
under-educated groups.
10) Conclusion
As we conclude our discussion on
measles, we'd want to extend our heartfelt appreciation to all of our readers
who have joined us on this trip. Your enthusiasm and participation have made
our investigation of a crucial public health issue both meaningful and
enjoyable.
We've discussed the history of
measles, its symptoms, and the serious problems it may cause. We've also
emphasized the incredible progress achieved in combatting this disease since
the introduction of the measles vaccine in 1963, as well as the dedicated
efforts of health professionals, policymakers, and parents all across the
world.
Our investigation, however, has
highlighted the persisting problems in the fight against measles. Measles
remains a concern, despite the availability of a safe and effective vaccine,
particularly in places with poor vaccination rates. Maintaining high
vaccination coverage is critical since it not only protects individuals but
also contributes to the larger objective of herd immunity.
We hope that this blog series has
given you useful information and increased your awareness of measles and the
necessity of immunization. We feel that knowledgeable readers like you play an
important role in raising awareness and dispelling myths regarding
vaccinations.
Thank you once more for your time
and interest. We hope to continue providing you with interesting and
thought-provoking information in the future. Stay well, stay educated, and keep
in mind that every vaccine helps in the battle against avoidable illnesses such
as measles.
FAQ’s
Measles is a highly contagious
disease caused by a virus. It can lead to serious complications such as
pneumonia, brain damage, blindness, deafness, and even death, especially in
young children and adults
Measles spreads through the air
when an infected person breathes, coughs, or sneezes. The virus can survive in
small droplets in the air for several hours. You can become infected when you
breathe in these droplets or touch objects contaminated with the virus
3) What are the symptoms of measles?
Symptoms of measles include
fever, cough, runny nose, red and inflamed eyes, loss of appetite, and a rash
that usually starts on the face and neck and spreads to the rest of the body
Measles is diagnosed by a
combination of the patient’s symptoms and laboratory tests. Detection of
measles-specific IgM antibody in serum and measles RNA by real-time polymerase
chain reaction (RT-PCR) in a respiratory specimen are the most common methods
for confirming measles infection
5) Is there a treatment for measles?
There is no specific antiviral
treatment for measles. Management of the disease includes hydration, fever
control, and vitamin A supplementation. If you have been exposed to the measles
virus and have not had the disease or received 2 doses of a measles vaccine,
you should get immunized to prevent the illness
6) How can measles be prevented?
The best protection against
measles is vaccination. The measles, mumps, and rubella (MMR) vaccine is safe
and highly effective
7) Who should get the measles vaccine?
The measles vaccine is
recommended for everyone age 1 year and older. Certain adults are at higher
risk of exposure to measles and may need a second dose of MMR unless they have
other evidence of immunity
8) What if I have been exposed to measles?
If you have been exposed to the
measles virus and have not had the disease or received 2 doses of a measles
vaccine, you should get immunized to prevent the illness. You need to get the
vaccine within 72 hours after exposure in order to be protected against the
measles virus
9) Can someone get measles more than once?
No, once a person has had
measles, they are immune for life
10) What are the complications of measles?
Complications of measles can
include ear infections, diarrhea, pneumonia, and encephalitis (brain
inflammation). Complications and death are most common in infants less than 12
months of age and in adults
11) How common is measles in the United
States?
Before the measles vaccine was
licensed in 1963, there were an estimated 3–4 million cases each year. Since
2000, when measles was declared eliminated from the U.S., the annual number of
cases has ranged from a low of 37 in 2004 to a high of 1,282 in 2019
12) Can measles be eradicated?
Yes, it's possible. The first
step is to eliminate measles from each country. High sustained baseline measles
vaccine coverage and rapid public health response are critical for preventing
and controlling measles cases and outbreaks
13) What should I do if I think I have measles?
If you have fever and a rash and
think you may have measles, especially if you have been in contact with someone
with measles or traveled to an area with a measles outbreak, have yourself
examined by a health care provider. It is best to call ahead so that you can be
seen quickly and without infecting other people
14) How can I prevent spreading measles to
others?
If you have measles, you can help
prevent spreading it to others by staying at home for at least 4 days after the
rash first appeared, washing your hands regularly, coughing or sneezing into a
tissue or sleeve rather than your hands, and not sharing food, drinks, or
cigarettes, or kissing others
15) Is measles more severe in certain
populations?
Yes, measles can be especially
severe in persons with compromised immune systems. Measles is more severe in
malnourished children, particularly those with vitamin A deficiency
16) What is the home treatment for measles?
Home treatment for measles
includes rest, hydration, fever control, and isolation to prevent spread to
others
17) Can measles lead to death?
Yes, death from measles occurs in
2 to 3 per 1,000 reported cases in the United States. In developing countries,
the fatality rate may be as high as 25%
18) Are there any side effects of the
measles vaccine?
Side effects of the measles
vaccine are usually mild and temporary, such as a fever or rash. More severe
reactions, including allergic reactions, are rare
19) Can measles still be a threat in the
United States?
Yes, since measles is still
common in many countries, travelers will continue to bring this disease into
the United States. Measles is highly contagious, so anyone who is not protected
against measles is at risk of getting the disease
20) What is the global impact of measles?
Measles is a leading cause of
death among children worldwide. Outbreaks in countries to which Americans often
travel can directly contribute to an increase in measles cases in the United
States










Comments
Post a Comment